Patient Info
Structure of female reproductive system
- Genitals
- Structural Features of Vagina
- Functions of Vagina
- Vaginal Micro flora
- Composition of Normal Vaginal Flora
- Species composition of Vaginal Microflora
Female reproductive system includes the genitals, mammary glands, and the endocrine glands regulating the work of genitals. These organs are involved in the main mission of the woman which is childbirth. Female reproductive structures include parts inside and outside the body and are divided into internal and external depending on whether they are located within the pelvis (the lower abdominal cavity) or outside the pelvis.
GENITALS
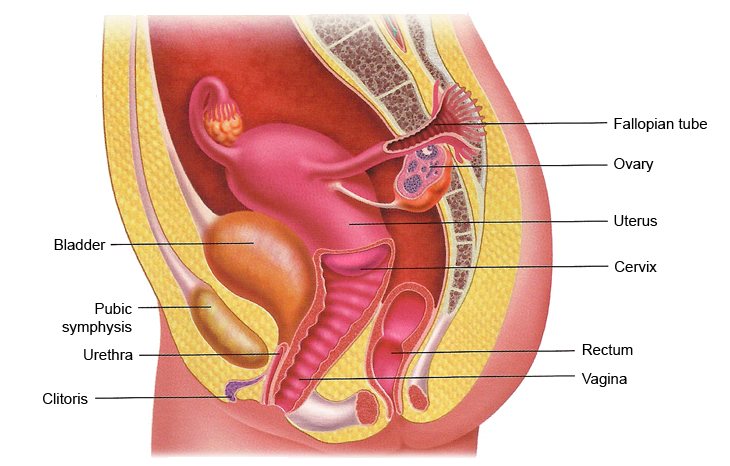
External genitals consist of pubis, large and small labia [lips], the clitoris, the vagina, the hymen (a border between the internal and external genitals).
The internal genitals includes vagina, uterus and its appendages (fallopian tubes and ovaries), as well as connective tissue and smooth muscle formation, which functions in fixing the uterus position.
Let’s find out what is vagina.
STRUCTURAL FEATURES OF VAGINA
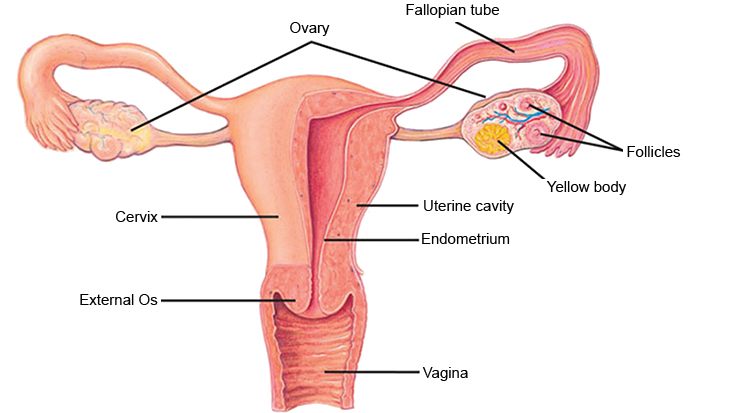
Vagina is a hollow elastic muscular tube, kind of a channel that connects the area of external genitals (vulva) and uterus. The average length of vagina varies from 7 to 12 cm, the size of the Vagina differs slightly in each woman, it is more individual. When woman stands, vagina is slightly bended upwards, without taking any vertical or horizontal position.
The walls of vagina consist of three layers with total thickness of 3-4 mm:
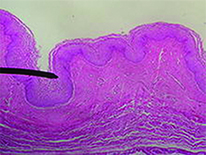
Internal layer. This is vaginal mucosa. It is covered with stratified squamous epithelium, which forms many folds in the vagina (look at the picture, vagina seems tubular). When necessary vagina can change its size and stretch due to these folds.
Middle layer. This is smooth muscle layer of the vagina. Muscles are mostly longitudinal, but can have also circular direction. In its upper part, vaginal muscles transform into the uterine musculature. In the lower part of the vagina it becomes more durable, gradually connecting with the muscles of perineum.
Outer, or adventive layer. It is composed of loose connective tissue and components of muscle fibers.
Vaginal walls are divided into front and rear, connected one with another. The upper end of the vaginal wall covers the cervix, separating the vaginal part and forming so-called vaginal vault in the area around.
The lower end wall opens into the vagina threshold. Threshold of virgins is closed by hymen.
As we said before, the vagina is elastic, it can stretch during intercourse and during childbirth to allow the fetus to leave (up to 10 – 12 cm in diameter). This is possible thanks to the middle smooth muscle layer. In its turn, the outer layer (consisting of connective tissue) connects vagina with adjacent organs – Urinary bladder and the rectum, which are respectively located in front and behind the vagina.
The inner walls of the vagina are covered with special mucus secreting glands. This mucus has a white colour and typical smell, and slightly acid reaction as well. Mucus moisturizes healthy vagina and clears it from so called “biological garbage” – bodies of dead cells, bacteria. Due to its acidic reaction, mucus prevents development of many pathogenic microbes. Normally, mucus is discharged from vagina in very small quantities.
Normally vagina should be moisturized all the time. It helps not only to maintain a healthy micro flora, but also ensures completeness during sexual intercourse. Estrogen hormones regulate the process of vaginal secretion. During menopause, production of hormones decreases sharply, due to this decrease of production woman can feel vaginal dryness and pain during sexual intercourse.
Typically, the vaginal walls have pale pink color, but while pregnancy they become brighter and darker. Furthermore, the vaginal walls have body temperature and are soft to touch.
FUNCTIONS OF VAGINA
Sexual function
The main function of the vagina is participating in the process of conceiving children: the seminal fluid, produced during intercourse, gets into vagina where sperm penetrate into the uterus and tubes. Sperm accumulates mainly in the back (the deepest) vault of the vagina, which is bordered by the cervix. Usually cervical canal is firmly plugged with mucus plug, but during ovulation in women, the egg cell leaves the ovary, the mucus becomes less viscous, allowing the sperm to overcome the cervix and to reach the egg cell, to cause fertilization and give rise to new life.
Childbirth function
Vagina together with the cervix forms the birth canal where the baby moves through from uterus. During pregnancy vaginal tissues change under the influence of hormones, vaginal walls become more elastic and can stretch so much as to smoothly bring the fetus out.
Protective function
Barrier function of the vagina and its ability to cleanse itself are also important. As we have said above, the inner part of the vagina is covered with layers of flat cells – stratified squamous epithelium, or mucosa. Mucosa is constantly wet due to glands that produce vaginal lubricant. The lubricant is a mixture of various biological fluids produced by the cervical mucus glands and the vaginal canal, the dead cells of the vaginal epithelium, and various microorganisms. It is transparent, has a neutral odor and acidic environment. Vaginal mucosa blocks the growth of pathogenic microbes.
The vagina has an important ability particularly to clean itself, or to regulate the stability of its environment. This process is regulated by the female hormones; estrogen and progesterone secreted by the ovaries. Under the influence of estrogen vaginal mucosa cells synthesize glycogen, the substance, which is then converted into lactic acid. The process of producing lactic acid from glycogen occurs with the participation of lactic acid bacteria (Doderlein bacillus) while the vaginal environment is maintained in an acidic condition, (pH ranged from 3.8 to 4.5).
Vaginal microflora is women’s main guard giving protection from genital infections. Vagina of healthy women contains mainly Doderlein bacillus and a small number of other microbes, including staphylococci, streptococci, yeasts, anaerobes. The acidic environment of healthy vagina does not allow reproducing of other microorganisms. Even gonorrhea and trichomoniasis stirrers can be present in small amounts in the vaginal microflora , not leading to development of infection.
Even now, there are women who do not understand genital hygiene. They practice vaginal washing with water or some solutions. In fact, this harms beneficial microorganisms in Vagina and does not help the woman. After all, nature gave to vagina the ability to cleanse itself.
Excretion function.
Vagina also serves as a kind of channel through which physiological discharges of vagina and cervix are excreted. Healthy women have up to 2 ml of excretions per day, but their amount can vary depending on the phase of menstrual cycle.
VAGINAL MICROFLORA
Like other organs of the body which have contact with the external environment (e.g., mouth, nose), vagina of healthy women is not sterile, and populated by numerous microbes that form so-called normal vaginal microflora.
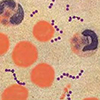
Characteristics of the vaginal microflora of adult women
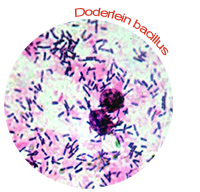
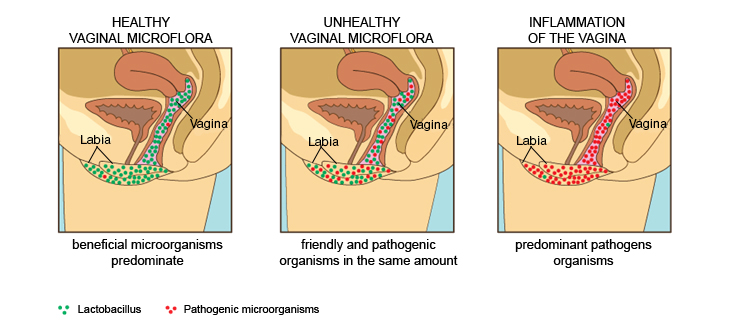
Normal microflora includes all organisms that are able to survive, develop and coexist in a particular physical environment, without causing disease of organism. Beneficial microorganisms predominate in vagina of healthy woman. Leading among them are lactobacilli (Doderlein bacillus) – microscopic bacteria that produce hydrogen peroxide and form a barrier to the spread of pathogens (disease-causing) microbes. In addition, lactic acid produced during their life largely determines the acidity (pH) of vaginal environment. With enough lactobacillus, vaginal acidic environment inhibits the growth of pathogenic bacteria. Thus, the useful microflora protects vagina against microbes that might cause inflammation. If lactobacillus dies due to some reason, the acidity of the vaginal environment decreases and the number of pathogenic bacteria grows, causing development of vaginal dysbiosis.

Vaginal microflora composition determines also the composition of microflora of its two surrounding organs – the cervix and the urethra. During the evolution, a number of microorganisms adapted to life in the urogenital organs. Some of them peacefully coexists with the organism, reproduces and even performs a very necessary function. This is called the normal microflora (natural).
In addition to Doderlein bacilli, we can also find in the vagina of a healthy woman minor amounts of staphylococci, streptococci, Candida fungi and Ureaplasma can be detected. Thus, side by side with useful bacteria, lives bacteria with pathogenic properties, but these pathogenic properties are not able to show up until it is hampered by their helpful “neighbors”. With normal immunity, various microorganisms colonizing the vagina are in a “dormant” state. With the weakening of immunity favorable conditions for the expansion of pathogenic microbes appears.
Due to various gynecological diseases (including cases of sexually transmitted diseases) composition of vaginal microflora may change and it is possible to define the cause of disease by the nature of its changes.
Vaginal microflora in the period before puberty

The interesting fact is that the composition of the vaginal microflora of the woman is not constant during her life. Some scientists believe, for example, that immediately after girl’s birth her vagina is filled with mucus and therefore sterile. Only 3-4 hours after the birth lactobacilli, bifidobacteria and other microorganisms are detected in the vagina. According to experts, the microflora of girls’ genital tract is represented mainly by coccal flora; in vaginal smears, individual leukocytes and epithelial cells are determined. Basically it is microbes from the birth canal and from the skin of mother.
Approximately, from the age of 8-9 starts the puberty phase in girls. Starting from this period girls have mucous secretions. They are normally transparent, have no odor and are not disturbing. Microflora composition also changes: in 60% of cases lactobacillus are determined, vaginal environment becomes acidic, pH equal to 4 – 4.5.
From the adolescence, (16 years) girls’ vaginal microflora becomes same as flora of adult woman.
During menstruation, the total number and species composition of the microflora varies a little, but after its end vaginal microflora quickly returns to normal condition.
Changes in vaginal microflora in postmenopausal period

Women, who have reached the age of 45, start having some changes appear in their body. During the menopausal period, estrogen deficiency is progressing due to the depletion of the ovary. It causes the development of atrophic age- related changes in the urinary mucosa tract.The medical term for these changes is menopausal syndrome, but in everyday life they are often called as “climax”. The transition from adulthood to old age is a crucial time for women. First manifestations of menopause are menstrual irregularities, and then its termination. During menopause the ovaries gradually fade – stops maturation of the oocytes, a woman can no longer get pregnant.
During menopause production of female hormones estrogen decreases, which causes a gradual destruction of the urogenital tract mucosa. Urogenital disorders, including vaginal dryness, itching and burning, constantly emerging infections of vagina, chronic cystitis, urethral mucosa eversion, etc. are a direct result of atrophy of the vaginal mucosa.
Gynecologist can observe the disappearance of woman’s vaginal microflora and change of its pH during menopause. The destruction of the vaginal mucosa leads to decreasing of lactobacilli amount and reducing of lactic acid amount; gradually vaginal microflora changes to enterobacteria, mainly E. coli, and typical representatives of the skin microflora. Like in childhood, vaginal environment’s pH increases to 5,5-6,8 during menopause.
Vaginal microflora during pregnancy
 During pregnancy, hormonal background of woman changes and it directly affects the “inhabitants” of the vaginal mucosa. The production of lactic acid increases, and therefore number of fungi Candida albicans is increasing, which cause urogenital candidiasis (or Vaginal thrush). Normally, increase in their amount is asymptomatic, does not cause discomfort to woman and immediately after childbirth number of bacteria and fungi decreases to normal. But in approximately 20% of cases Candida albicans cause the development of inflammation of various severities, pregnant women often complain to discomfort, burning sensation in vagina and urinary tract. Treatment of these inflammations is complicated cause of the toxic effects of most antifungal drugs on the fetus. This issue remains unsolved, the effective specific agents that are safe for the systematic (and local) administration for pregnant women, unfortunately, does not exist.
During pregnancy, hormonal background of woman changes and it directly affects the “inhabitants” of the vaginal mucosa. The production of lactic acid increases, and therefore number of fungi Candida albicans is increasing, which cause urogenital candidiasis (or Vaginal thrush). Normally, increase in their amount is asymptomatic, does not cause discomfort to woman and immediately after childbirth number of bacteria and fungi decreases to normal. But in approximately 20% of cases Candida albicans cause the development of inflammation of various severities, pregnant women often complain to discomfort, burning sensation in vagina and urinary tract. Treatment of these inflammations is complicated cause of the toxic effects of most antifungal drugs on the fetus. This issue remains unsolved, the effective specific agents that are safe for the systematic (and local) administration for pregnant women, unfortunately, does not exist.
COMPOSITION OF NORMAL VAGINAL FLORA
Normal vaginal microflora of healthy women of reproductive age contains a wide variety of bacterial species. In general, all these microorganisms can be divided into 2 groups, aerobic (they need oxygen for existence) and anaerobic (can grow without oxygen).
General characteristics of the vaginal flora can be determined by a special analysis – floral smear.
Normal smear imply the presence of the following indicators:
Squamous epithelium – the layer of cells lining the vagina and cervix. Normally epithelium must be present in smear. If smear does not contain epithelium, then the gynecologist has reason to assume lack of estrogen, as due to excess of male hormones. Lack of squamous epithelium in the smear shows atrophy of epithelial cells. Large number of squamous epithelium – a sign of inflammation.
Leukocytes in smear. The norm is up to 15 units in sight. A small amount of leukocytes in smear is normal as leukocytes have a protective function, preventing penetration of infection to woman’s genitals. Increased amount of leukocytes in smilar usually is observed during inflammation of vagina (colpitis, vaginitis). The more leucocytes are in smear, the worse is the disease.
Staphylococcus aureus in small quantities is considered as normal. Significant increase of Staphylococcus in smear, is smilar to leukocytes increase, can be a symptom of inflammation of vagina or uterine mucosa (endometritis).
Bacillus forms a normal vaginal flora. There should not be any other microorganisms except bacillus in smear.
Gynecological smears may contain heterogenous microorganisms that indicate the presence of infection in smear. Results of smear can show the contents of the following bacteria:

Cocci – unlike bacillus, these are spherical bacteria. In addition to cocci, the results of smear may contain diplococci – double bacillus or gonococci – a symptom of gonorrhea.

Small bacillus in smear – these are most often gardnerella – are pathogens of gardnerellosis or bacterial vaginosis.
“Key” cells in smear (abnormal cells) are squamous epithelial cells, glued with small bacillus. As with gardnerella, if smear contain abnormal cells, the doctor can make a diagnosis – vaginal dysbiosis.

Fungus in smear is a sign of candidosis. While latent (asymptomatic) stages of thrush fungus can be found in the form of spores.

If vaginal smear results indicate the presence of trichomonade, the doctor has all the reasons to suppose that patient has trichomoniasis.
Even if the results of smear show the presence of cocci, small bacillus and “key” cells, Pap smear alone is insufficient for diagnosis of bacterial vaginosis. Most likely, the gynecologist will require to make a bacteriological swab and DNA diagnostics (smear by PCR method).
Why smear results are not enough for accurate diagnosis of sexually transmitted diseases (STDs)?
Doctors explain it with the following reasons:
- Viral, chlamydial, mycoplasma and ureaplasma infection are hardly defined in the urogenital smear. Viruses, chlamydia, ureaplasma and mycoplasma organisms have very small size, that is why they are difficult to see under a microscope during normal smear analysis. For the diagnosis of these infections, there are other more informative methods (smear PCR, ELISA diagnostics).
- Fungus discovered in a smear is a true sign of vaginal thrush. But candidiasis may be a recurrent disease, which developed on the background of a more serious sexually transmitted infection.
- Increased leukocytes in smear may be the result of misdiagnosis because of accidental exposure of pus when taking smear. Large amount of leukocytes in smear prevents technician to “see” STD pathogen.
In many cases, the vaginal smear reveals infection, but not “the nature” (pathogen) of the infection. And very important – it is impossible while using smear to find out the sensitivity of these pathogens to certain antibiotics. This problem can be solved by taking a swab for studying the flora.
SPECIES COMPOSITION OF VAGINAL MICROFLORA
Studying the flora is needed in order to determine the species composition of vaginal flora (i. e., what bacteria species “inhabit” the vagina). This study helps not only to identify activators of disease, but also to learn its number and drugs to which they are sensitive (antibiogram).
Normally, lactobacilli (Doderlein bacilli) have the highest concentration in the microflora, the number of them may reach 109 CFU/ml. We already talked about important role of lactobacilli in protection of female genital organs from infection. Thus, the presence of lactobacilli and their number are the determinants of vaginal flora condition.

Bifidobacteria are also part of the normal vaginal microflora. Vagina of healthy woman has nearly 103 – 107 CFU/ml of them. Like lactobacilli, they are involved in maintaining an acidic environment in vagina. Moreover, bifidobacteria produce amino acids and vitamins, which are actively used by the human body in its metabolism.

Peptostreptococci are the third component of the normal flora (Doderlein flora). Their number should be 103 – 104 CFU/ml. Despite the fact that peptostreptococci are a part of the normal flora of female genital organs, they can be often found in cases of septic abortion, tubal-ovarian abscesses, endometritis and other hard infections of female genitals.In addition, peptostreptococci together with other pathogenic microorganisms are found in case of bacterial vaginosis.

Propionobacterium produce organic acids and that is why they have immunostimulating properties. Their quantity should not exceed 104 CFU/ml.
Number of gardnerellas often reaches 106 CFU/ml. G. vaginalis are pathogens of bacterial vaginosis.

Corynebacterium are found in the amount of 104 – 105 CFU/ml in vaginas of healthy women. Genital Mycoplasma, Staphylococcus occurs in amount of not more than 104 CFU/ml.
Number of streptococci in vaginal discharge varies considerably and according to different sources can be 104 – 105 CFU/ml. Enterococci are often found while inflammatory diseases of the urogenital system.
-
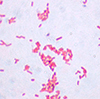
Enterobacteria E. coli, Proteus spp., Klebsiella spp., and P. aerugenosa, which are found in amount 103 – 104 CFU/ml, can cause urogenital infectious diseases.

Candida Fungi can be determined in amount up to 104 CFU/ml without causing inflammation. Number of fungi may increase during pregnancy.
